| |
FONTE, Cristina1
COIMBRA, Filipe.2 1.Dentist, Faculty of Dental Medicine, University of Porto, acristinafonte@hotmail.com; 00351938536255
2. Associate Professor, Faculty of Dental Medicine, University of PortoAbstract: This is a clinical case in which a swelling located in the mandible was observed that involves the bony cortical located in the horizontal branch of the mandible on the right side, with no symptoms or typical signs of inflammation, there is a need to make the differential diagnosis between benign and malignant tumor, for which a CT scan and an incisional biopsy were performed. The results of these tests rule out malignancy and suggest that it is a peripheral ossifying fibroma. Keywords: ossifying fibroma, fibrous dysplasia, fibro-osseous lesions Introduction
A swelling of the cortical bone observed in the clinical examination in any of the jaws and in which in the radiographic examinations, dark (radiolucent) and light (radiopaque) images are observed can represent several pathologies that occur when bone is replaced by fibrous tissue with newly mineralized material.(1-4) The initial diagnosis is intended to exclude malignancies, since they are the most aggressive and can jeopardize the lives of patients. Within the benign pathologies we must differentiate: the developmental changes known as fibro-osseous dysplasias and cemento-osseous dysplasias, the reactive or dysplastic processes, commonly diagnosed as idiopathic osteosclerosis whose differential diagnosis includes focal sclerosing osteomyelitis, and the benign neoplasms, represented for the most frequent benign tumors whose example is ossifying fibroma.(5, 6) The most common ones found in the maxillary bones are fibrous dysplasias, ossifying fibroma and cemento-osseous dysplasias.(1, 5)
Idiopathic osteosclerosis represented on the X-ray as a whitish zone is an intraosseous growth, located, with production of compact bone tissue in the maxillary bones, it is more frequent in the molar and premolar area.(7) It is a benign, unilocular pathology and non-expansive, with unknown etiology, it is essential to perform specific radiographic examinations (computed tomography) to differentiate it from a root rest, from condensing osteitis, from apical cement-bone dysplasia, from ossifying fibromas, from osteomas, osteoblastomas and cementoblastomas.(7) In some situations, anatomopathological examination is necessary to arrive at the correct diagnosis.
Sclerosing osteomyelitis represents a suppurative infectious process, which induces the immune system to respond to an infectious agent, and can present the typical signs and symptoms of inflammation. Radiographically it looks like snowflakes or cotton, that is, radiopaque areas surrounded by radiolucent halos.(8)
Ossifying fibromas are benign tumors of slow development, more frequent in the mandible (70-90% of cases (9)).(10-14) This tumor is composed of very cellular fibrous tissue with different percentages of bone or cement, similar to calcified tissue (15), which can be caused by stimuli, such as extractions or trauma (16).
Initially, ossifying fibromas are small and have radiolucent images, as they grow and mature they become radiolucent-radiopaque and later totally radiopaque (16-18), with their individual radiographic particularity being the clear circumscription of adjacent structures (19). Its expansion is slow, asymptomatic and symmetrical from the epicenter, forming a spherical or ovoid mass visible on the X-ray and TC.(11, 20) They can reach disfiguring sizes due to their slow and painless growth.(10, 11, 14) The displacement of teeth may be the only clinical sign, and the adjacent teeth remain vital, root resorption is rare.(11)
It is more frequent in women between 20 and 30 years old, however it can appear at other ages.(13, 14, 17, 21, 22) They appear in the branch of the mandible or above the alveolar bone in the maxilla, mainly in the dental support area, where there is a greater induction of bone and cement,(10) being frequent in the area of premolars and mandibular molars.(1, 10, 19, 23-26)
Histologically, ossifying fibromas are made up of fibrous tissue with different degrees of cellularity and mineralized material, where the hard tissue may present in the form of osteoid trabeculae and bone or cement, looking like sparsely cellular spherical spherules.(10) Spheres of material are also observed identical to the cementum with diffuse peripheral edges in the adjacent connective tissue, intralesional hemorrhage being unusual.(27)
Resection is indicated when the lower border (1 cm), the maxillary sinus or nasal cavities are reached, and the encapsulation disappears generally, the result of enucleation is the same as that of resection, since this lesion does not infiltrate more than 1 or 2 mm from the edge, so the resection margins do not reach more than 5 mm.(10) If enucleation and curettage is performed, it is recommended normal bone regeneration since other materials delay healing.(10) Regardless of the therapy method, the percentage of recurrence is almost non-existent, however periodic control is necessary. (10) Case Report
Asymptomatic female patient, 49 years old, with no noticeable clinical signs. It was observed in the Dental Medicine consultation with complaints of swelling located in the mandibular region. On periapical X-rays, a radiopaque image with a radiolucent border was observed. The image was located in the posterior region of the third quadrant.
The extraoral examination (fig.1) does not reveal any changes in the mandibular region. In the intraoral examination, an expansion of the cortices is noted in the area of the 2nd premolar and lower molars (fig.2), without tooth displacement or soft tissue changes.  Fig.1 Extraoral examination without alteration of the mandibular region  Fig.2 Intraoral examination, slight expansion of corticals in the 2nd premolar and molar area Computed axial tomography (CT) was performed, which allowed us to verify that the swelling was radiopaque with a radiolucent halo, well-defined edges, measuring about 1.5 cm wide by 2 cm high, it was close of the cortex without reaching it, nor reaching the lower alveolar nerve (fig.3). No dental pieces were involved.  Fig.3 TC - well-defined edges with cortical proximity Both clinical observation and radiographic images suggested benignity since the tumor was well delimited and did not invade neighboring structures. The most likely differential diagnoses were as follows: fibro-osseous dysplasias, idiopathic osteosclerosis, focal sclerosing osteomyelitis, ossifying fibroma.
As the image was suggestive of tumor lesion, an incisional biopsy was performed for histological diagnosis. The result was ossifying fibroma, due to the presence of fragments of trabecular bone associated with the proliferation of fibroblasts, with foci of dystrophic calcification and without signs of malignancy (fig.4).  Fig.4 Fragments of trabecular bone associated with fibroblast proliferation, with foci of dystrophic calcification The patient was referred to a Hospital Santo António for maxillofacial surgery where a second incisional biopsy was performed, where a spindle cell neoplasm with bone trabeculae was observed wavy without mitosis or atypical nucleus-cytoplasm. (fig.5) In the histological diagnosis it was suggested that it was a fibrous dysplasia.
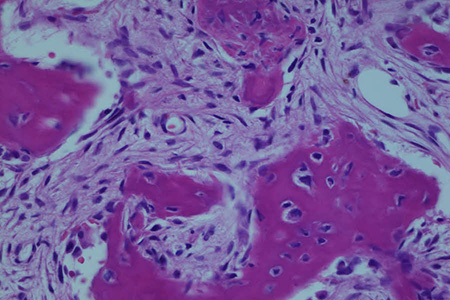
Fig. 5 Spindle cell neoplasm with wavy bone trabeculae without mitosis or atypical nucleus-cytoplasms Strict patient control was recommended to assess possible changes.
Discussion
In clinical observation, the possibility of several differential diagnoses compatible with the observed bone swelling was raised: ossifying fibroma, fibrous dysplasia, osteoblastoma, odontogenic cysts, calcifying epithelial odontogenic tumor and calcifying odontogenic cyst. When we look at X-rays and CT, we rule out the possibility that it is a cementoblastoma and exclude periapical cement-bone dysplasias since there was no relationship between the tumor and neighboring teeth.(30, 31) We excluded the possibility of sclerosing osteomyelitis due to the absence of inflammatory signs and symptoms.(8) The images also made it possible to exclude the cysts, as there was no central radiolucent zone and sclerotic halo around the lesion.(32) The non-invasion of neighboring structures observed in CT and preservation of the cortical bone and the fact that the tumor is well delimited did not suggest malignancy, so the diagnosis of sarcoma was ruled out, however only biopsy can provide the definitive diagnosis.(33) Osteoblastoma, which was one of the diagnostic possibilities, was ruled out since there was no pain symptom typical of this pathology.(34)
In the differential diagnoses, we maintained the possible fibrous dysplasia and the ossifying fibroma. The result of the two biopsies was identical in the description of the cell structures observed and definitively ruled out the possibility of it being a malignant tumor. However, the diagnosis of the first biopsy was of ossifying fibroma, while that of the second was of bone dysplasia. This is partly understood by the cellular alterations being identical in one case and in the other, since bone substitution occurs by increased proliferation of cellular fibrous connective tissue mixed with irregular bone trabeculae.(11, 35) However, the images observed on CT scan reveal margins that are confused with adjacent normal bone, preventing the definition of the lesion limits without however reaching the cortical bone.(36)
Ossifying fibroma has centrifugal growth, also increasing in all directions, appearing with a well-circumscribed round appearance.(23) This rounded shape and the fact that it remains isolated from the cortical without involving it allows it to be distinguished from the bone dysplasia that is shaped ovoid and involves both the cortical bone and the medullary bone without a transition between the two. In our case, the type of rounded image is very suggestive of that of ossifying fibroma and in many cases serves for differential diagnosis. When lesions occur in the mandible and affect the lower margin, they can cause an upper deviation of the lower alveolar canal. (38, 39) In this case there is no such departure. Although ossifying fibroma has a specific radiological aspect, it can also show an irregular shape when it grows quite quickly.(9, 37)
Histologically, fibrous dysplasias are characterized by irregular immature bone trabeculae in a loose fibrous cellular network (disconnected, with a curvilinear shape).(5) These characteristics were not observed in this case. Ossifying fibroma, on the other hand, presents a more uniform pattern instead of a disorganized mixture of immature bone, lamellar bone and rounded particles,(5) which is in accordance with the biopsy performed.
The treatment option for ossifying fibroma varies depending on the size of the lesion, with curettage or enucleation being more frequent. Bone graft resection may be an option when there is an aggressive and recurrent lesion, however a similar low recurrence rate has been studied in both therapies.(42) In our case, follow-up was recommended due to the reduced tumor size. The most frequent clinical sign is asymmetry of the face with cortical expansion, (11) but in this case there is no asymmetry, as seen in fig1. Conclusion
Ossifying fibroma and fibrous dysplasia are the most frequent fibro-osseous lesions of the head and neck. Due to their similarities, it is essential to make a rigorous differential diagnosis to define the most suitable treatment method. References
1. Mortazavi H, Baharvand M, Rahmani S, Jafari S, Parvaei P. Radiolucent rim as a possible diagnostic aid for differentiating jaw lesions. Imaging Sci Dent. 2015;45(4):253-61.
2. Akbulut S, Demir MG, Basak K, Paksoy M. Maxillectomy for Cementifying Osseous Dysplasia of the Maxilla: A Case Report. Acta Medica (Hradec Kralove). 2015;58(1):32-4.
3. Chennoju SK, Pachigolla R, Govada VM, Alapati S, Balla S. Idiosyncratic Presentation of Cemento-Osseous Dysplasia - An in Depth Analysis Using Cone Beam Computed Tomography. J Clin Diagn Res. 2016;10(5):ZD08-10.
4. de Noronha Santos Netto J, Machado Cerri J, Miranda AM, Pires FR. Benign fibro-osseous lesions: clinicopathologic features from 143 cases diagnosed in an oral diagnosis setting. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(5):e56-65.
5. Akashi M, Matsuo K, Shigeoka M, Kakei Y, Hasegawa T, Tachibana A, et al. A Case Series of Fibro-Osseous Lesions of the Jaws. Kobe J Med Sci. 2017;63(3):E73-E9.
6. Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol. 2008;2(3):177-202.
7. Fuentes R, Arias A, Astete N, Farfan C, Garay I, Dias F. Prevalence and morphometric analysis of idiopathic osteosclerosis in a Chilean population. Folia Morphol (Warsz). 2018;77(2):272-8.
8. Owlia F, Akhavan Karbassi MH, Mirjalili N, Taghipour Zahir S, Gholami N, Karimi S. A localized sclerosing osteomyelitis at the periapex of a vital tooth: report of a misdiagnosis. J Dent Res Dent Clin Dent Prospects. 2011;5(3):102-5.
9. Liu Y, Wang H, You M, Yang Z, Miao J, Shimizutani K, et al. Ossifying fibromas of the jaw bone: 20 cases. Dentomaxillofac Radiol. 2010;39(1):57-63.
10. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral & maxillofacial pathology. 3th ed ed. St. Louis: Saunders Elsevier; 2009. XVI, 968 p.
11. Katti G, Khan MM, Chaubey SS, Amena M. Cemento-ossifying fibroma of the jaw. BMJ Case Rep. 2016;2016.
12. Kharsan V, Madan RS, Rathod P, Balani A, Tiwari S, Sharma S. Large ossifying fibroma of jaw bone: a rare case report. Pan Afr Med J. 2018;30:306.
13. Dewan HS, Dewan SK, Bahl S, Tushar Parekh P. Cemento-ossifying fibroma of mandible mimicking complex composite odontome. BMJ Case Rep. 2016;2016.
14. Bala TK, Soni S, Dayal P, Ghosh I. Cemento-ossifying fibroma of the mandible. A clinicopathological report. Saudi Med J. 2017;38(5):541-5.
15. Hamner JE, 3rd, Scofield HH, Cornyn J. Benign fibro-osseous jaw lesions of periodontal membrane origin. An analysis of 249 cases. Cancer. 1968;22(4):861-78.
16. Galdeano Arenas M, Crespo Pinilla JI, Alvarez Otero R, Espeso Ferrero A, Verrier Hernandez A. Cemento-ossifying fibroma of mandibular gingiva: single case report. Med Oral. 2004;9(2):177-9, 6-7.
17. Ong AH, Siar CH. Cemento-ossifying fibroma with mandibular fracture. Case report in a young patient. Aust Dent J. 1998;43(4):229-33.
18. Mithra R, Baskaran P, Sathyakumar M. Imaging in the diagnosis of cemento-ossifying fibroma: a case series. J Clin Imaging Sci. 2012;2:52.
19. McCarthy EF. Fibro-osseous lesions of the maxillofacial bones. Head Neck Pathol. 2013;7(1):5-10.
20. Bertrand B, Eloy P, Cornelis JP, Gosseye S, Clotuche J, Gilliard C. Juvenile aggressive cemento-ossifying fibroma: case report and review of the literature. Laryngoscope. 1993;103(12):1385-90.
21. MacDonald-Jankowski DS. Ossifying fibroma: a systematic review. Dentomaxillofac Radiol. 2009;38(8):495-513.
22. Eversole LR, Merrell PW, Strub D. Radiographic characteristics of central ossifying fibroma. Oral Surg Oral Med Oral Pathol. 1985;59(5):522-7.
23. Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg. 1993;51(8):828-35.
24. Sarwar HG, Jindal MK, Ahmad SS. Cemento-ossifying fibroma--a rare case. J Indian Soc Pedod Prev Dent. 2008;26(3):128-31.
25. Akcam T, Altug HA, Karakoc O, Sencimen M, Ozkan A, Bayar GR, et al. Synchronous ossifying fibromas of the jaws: a review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(5 Suppl):S120-5.
26. Trijolet JP, Parmentier J, Sury F, Goga D, Mejean N, Laure B. Cemento-ossifying fibroma of the mandible. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128(1):30-3.
27. Koury ME, Regezi JA, Perrott DH, Kaban LB. "Atypical" fibro-osseous lesions: diagnostic challenges and treatment concepts. Int J Oral Maxillofac Surg. 1995;24(2):162-9.
28. Chatterjee A, Ajmera N, Singh A. Peripheral cemento-ossifying fibroma of maxilla. J Indian Soc Periodontol. 2010;14(3):186-9.
29. Endo Y, Uzawa K, Mochida Y, Nakatsuru M, Shiiba M, Yokoe H, et al. Differential distribution of glycosaminoglycans in human cementifying fibroma and fibro-osseous lesions. Oral Dis. 2003;9(2):73-6.
30. Pathak J, Hosalkar RM, Sidana S, Swain N, Patel S. Benign cementoblastoma involving left deciduous first molar: A case report and review of literature. J Oral Maxillofac Pathol. 2019;23(3):422-8.
31. Brody A, Zalatnai A, Csomo K, Belik A, Dobo-Nagy C. Difficulties in the diagnosis of periapical translucencies and in the classification of cemento-osseous dysplasia. BMC Oral Health. 2019;19(1):139.
32. Bhat A, Mitra S, Chandrashekar C, Solomon M, Kulkarni S. Odontogenic cysts and odontogenic tumors in a large rural area from India. A 10-year reflection. Med Pharm Rep. 2019;92(4):408-12.
33. van den Berg H, Schreuder WH, de Lange J. Osteosarcoma: A Comparison of Jaw versus Nonjaw Localizations and Review of the Literature. Sarcoma. 2013;2013:316123.
34. Bokhari K, Hameed MS, Ajmal M, Togoo RA. Benign osteoblastoma involving maxilla: a case report and review of the literature. Case Rep Dent. 2012;2012:351241.
35. Raubenheimer EJ, Noffke CE, Boy SC. Osseous Dysplasia with Gross Jaw Expansion: A Review of 18 Lesions. Head Neck Pathol. 2016;10(4):437-43.
36. Nair SN, Kini R, Rao PK, Bhandarkar GP, Kashyp RR, Rai M, et al. Fibrous Dysplasia versus Juvenile Ossifying Fibroma: A Dilemma. Case Rep Dent. 2016;2016:6439026.
37. Wenig BL, Sciubba JJ, Cohen A, Goldstein MN, Abramson AL. A destructive maxillary cemento-ossifying fibroma following maxillofacial trauma. Laryngoscope. 1984;94(6):810-5.
38. Vura NG, Gaddipati R, Ramisetti S, Kumara R, Reddy R, Kanchi U. Surgical Management of Ossifying Fibroma in Maxilla: Report of Two Cases. J Int Oral Health. 2015;7(6):115-8.
39. Gnanadeepam S, Ponniah I. Ossifying fibroma with non-specific cystic degeneration: a case report. Oral Maxillofac Surg. 2012;16(1):101-5.
40. Prado Ribeiro AC, Carlos R, Speight PM, Hunter KD, Santos-Silva AR, de Almeida OP, et al. Peritrabecular clefting in fibrous dysplasia of the jaws: an important histopathologic feature for differentiating fibrous dysplasia from central ossifying fibroma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(4):503-8.
41. Shi RR, Li XF, Zhang R, Chen Y, Li TJ. GNAS mutational analysis in differentiating fibrous dysplasia and ossifying fibroma of the jaw. Mod Pathol. 2013;26(8):1023-31.
42. Eversole LR, Leider AS, Nelson K. Ossifying fibroma: a clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol. 1985;60(5):505-11.
|
 Información General
Información General Artículos
Artículos Notícias
Notícias Enlaces
Enlaces Contactar
Contactar Buscar
Buscar Premio Nadal
Premio Nadal Formación Continuada
Formación Continuada